Over the last few years, it has been recognized in the medical literature that conservative treatment works best for many cases of lumbar disc herniation. For patients with far-lateral, or extreme lateral herniation, however, the effectiveness of conservative care is less certain. This recent case study looked at the outcomes of nonsurgical management of a client with far-lateral disc herniation.
The 60-year-old male client was physically active, and had been seen at a Spine Specialty Center previously for treatment for lower back pain, which resolved. 15 months later, he presented at the Center again with severe back pain (present for 3 weeks), with pain radiating to his right buttock and calf.
Presenting Symptoms:
- Score of 73 (out of 100) on the Oswestry Low Back Questionnaire, and Numerical Pain Ratings of 6 (best) to 10 (worst) on a 1-10 scale.
- Difficulty transitioning from sitting to standing
- Altered gait
- Inability to assume erect position
- Lateral list to left
- Asymmetric static pelvic landmarks (right iliac crest 4 degrees high posteriorly, 2 degrees high anteriorly with standing).
- Pain on right side with lateral and backward bends
Initial treatment included manipulation, traction, and passive movements. This was followed up by instruction in self-correction exercises to be followed at home.
Follow-up consisted of:
2 days later: More traction/passive movement and gradual increase in weight bearing, and the patient was fitted with a back brace.
6 days later: manipulation was performed and the patient returned to work part-time. A MRI and surgical consult were also requested during this fourth visit.
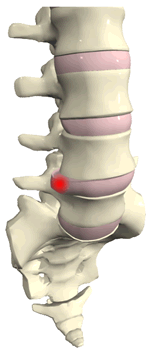
The lumbar MRI showed a lateral L5, S1 disc rupture with L5 nerve impingement; due to patient improvement, surgery was deferred. The patient was at work full-time, with his primary complaint sitting intolerance. With consultation, 1 week later a CT-guided transforaminal lumbar epidural and nerve root steroid injection were performed. Three days later, leg pain was reduced and the patient was sleeping better, was working full-time, and was driving.
The patient was then referred to physical therapy for further rehabilitation.
By the end of 4 weeks of physical therapy—8 weeks after being seen initially for the herniation—the patient had achieved scores of 0 on the Numeric Pain Scale, and of 2 (out of 100) on the Oswestry Low Back Pain Questionnaire.
During 2 follow-up visits at 14 weeks and 20 weeks after the initial complaint, all scores were 0. The patient was exercising by running or alternatively using a stair climbing machine with no pain, and continuing his stabilization exercises. He was asymptomatic 1 year later at follow-up.
The study authors also note that this patient responded well to nonsurgical intervention, but was very fit, motivated, and compliant with treatment. The case study did demonstrate the fact that a multi-disciplinary approach to treatment seems most effective: from manipulation and passive motion/traction, to epidural steroid injection once the effectiveness of these first interventions had plateaued, followed up by physical therapy and ongoing exercises.
Erhard RE, Welch WC, Liu B, Vignovi M. Far-lateral disk herniation: case report, review of the literature, and a description of nonsurgical management. Journal of Manipulative and Physiological Therapeutics 2004;27:e3.